[Ubicomp 23] Contact Tracing
CATCH is a contact tracing system for healthcare workers in hospital ICUs, using BLE beacons and room-specific localization methods.
TL;DR:
The CATCH (ContAct TraCing for Hospitals) system is an automated contact tracing solution designed to ensure the safety of healthcare workers in high-risk ICU environments. Using Bluetooth Low Energy (BLE) beacons, it tracks close contacts without smartphones, preserving privacy and reducing infection risks from mobile devices.
CATCH adapts to ICU layouts with specialized methods—such as Clustering for hallways and Semantic Localization for structured rooms. Real-world testing demonstrates CATCH’s high accuracy, providing a reliable, scalable solution that enhances infection control and reduces the need for manual contact tracing in hospitals. (Zhang et al., 2023)
Paper published in: 2023 ACM international joint conference on Pervasive and Ubiquitous Computing (UbiComp 2023) October 8-12, 2023 Cancún, Mexico
Background
The COVID-19 pandemic underscored the need for effective contact tracing in healthcare settings. ICUs, where healthcare workers frequently interact in close proximity, pose unique challenges to contact tracing. Traditional manual methods are resource-intensive and lack accuracy, which CATCH addresses through automated BLE-based technology.
Significance CATCH provides a robust, real-time solution to mitigate infection spread by accurately tracking close contacts among healthcare workers in ICU settings. By employing BLE beacons, CATCH ensures continuous monitoring without relying on smartphones, protecting worker privacy and minimizing device contamination risks. This automated approach not only enhances infection control but also reduces the burden on healthcare administrators.
-
Aim 1: Development of Room-Level Localization and Specialized Contact Tracing Methods
Implement room-level localization to identify healthcare workers’ locations within the ICU, reducing the search space for contact tracing. This includes developing customized tracing methods tailored for diverse ICU areas like hallways, structured rooms, and open spaces. -
Aim 2: Real-World Deployment and Evaluation in ICU Settings
Deploy CATCH in a real ICU environment to validate its accuracy and reliability compared to traditional methods, measuring performance through sensitivity, specificity, and contact tracing accuracy.
Method
Step 1: Room-Level Localization
CATCH first identifies healthcare workers’ locations by sorting BLE signal strength from nearby anchors and using a voting system to localize each worker to a specific room. A threshold check and smoothing method further refine accuracy by filtering out inconsistent signals and ensuring stability in estimated locations.
Step 2: Room-specific Contact Tracing Methods
1. Hallways
Clustering Contact Tracing: This method groups healthcare workers based on BLE signal similarity to identify clusters of people moving together, such as during patient rounds. It’s designed to address the unique challenges of narrow hallway environments, where signal interference and reflections are common.
We use RBO method to compute the similarity score between each pair of users, and DBSCAN to detect the patient round team in the hallway.
-
RBO is a similarity measure commonly used for comparing two ranked lists. For example, assume there are three ranked lists: [‘anchor 1’, ‘anchor 2’, ‘anchor 3’, ‘anchor 5’], [‘anchor 1’, ‘anchor 2’, ‘anchor 3’, ‘anchor 4’], [‘anchor 5’, ‘anchor 2’, ‘anchor 3’, ‘anchor 4’]. The RBO similarity score between List 1 and List 2 is higher than that between List 2 and List 3, because the difference at the tail has a smaller weight than the top.
-
DBSCAN is a density-based clustering method robust to noise. It can discover clusters, within which the density is higher than that out of the cluster. We can consider the clinicians in the patient round form a cluster in the hallway, since their mutual distances are significantly smaller compared to others. Another benefit of DBSCAN is its ability to handle outliers, meaning that some users may not belong to any cluster. The concept of “outlier” matches our contact tracing scenario in the hallway, where only the clinicians participating in the patient round form a cluster, while other clinicians in the hallway are “outliers” in the cluster discovery process.
2. Structured Rooms (e.g., Nurse Stations)
Semantic (Location) Localization: This method uses known, fixed workstations or desks to provide discrete “semantic” locations rather than tracking continuous movement. It simplifies the localization process by focusing on specific points in the room.
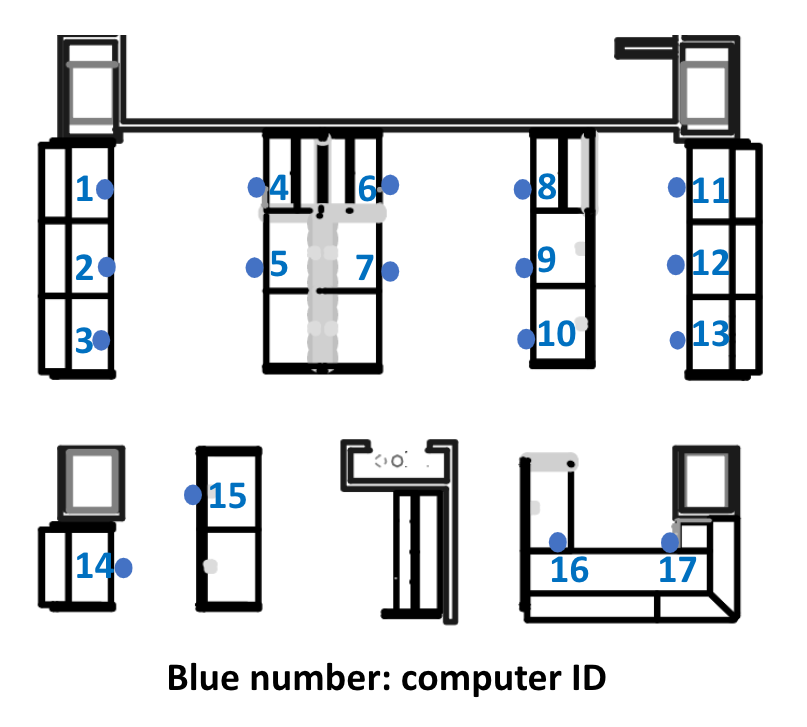
Graph-based Fingerprint: This approach improves location accuracy by using a graph-based analysis of BLE signal strength between nearby anchors, allowing it to differentiate between close workstations effectively.
In this graph signal framework, each anchor is represented as a node with an associated RSSI value. The graph’s structure is defined by a weighted adjacency matrix \(A \in \mathbb{R}^{M \times M}\), where each entry \(A_{ij}\) represents the edge between \(\text{Anchor}_i\) and \(\text{Anchor}_j\) based on their physical distance, \(w_{ij}\). The weight matrix \(\mathcal{W}\) is defined as:
\[\mathcal{W}_{ij} = \exp\left(-\frac{w_{ij}^2}{2\sigma^2}\right)\]The adjacency matrix \(A\) is then calculated as:
\[A_{ij} = \begin{cases} 0 & \mathcal{W}_{ij} \leq \beta \\ \mathcal{W}_{ij} & \text{otherwise} \end{cases}\]An edge with a smaller weight indicates greater physical distance between anchors. For anchors that are far apart, \(A_{ij} = 0\) (no edge). The diagonal degree matrix \(D\), representing the sum of each node’s edges, is computed as: \(D_{ii} = \sum_j A_{ij} \in \mathbb{R}^{n \times n}\) With \(A\) and \(D\), the Laplacian matrix \(L\) is defined as: \(L = D - A \in \mathbb{R}^{n \times n}\).
Using the RSSI vector \(x_i \in \mathbb{R}^n\), the product \(L\textbf{x}\) captures local variations of node values relative to connected nodes, enhancing location differentiation. The input vector for the KNN model becomes \([\textbf{x}, L\textbf{x}]\), which incorporates these local signal variations for improved localization accuracy. Hyperparameters \(\sigma\) and \(\beta\) are optimized using grid-search cross-validation.
-
The term \(L\textbf{x}\), the graph Laplacian transformation of the RSSI vector \(\textbf{x}\), captures local variations in signal strength by comparing each anchor’s RSSI to the average of its neighbors.
\[Lx = \left[ \sum_{j=1}^{n} A_{ij} (x_i - x_j) \right]_{\text{for each } i} \in \mathbb{R}^{n}\]This transformation gives higher weights to the difference of nearby anchors, which may in theory receive similar RSSI values, for finer differentiation to enhance localization accuracy by emphasizing “local” signal differences.
3. Open Spaces (e.g., Break Rooms, Conference Rooms)
- Radio Fingerprint Localization: This traditional fingerprinting method estimates user positions by comparing BLE signals to a pre-established database, ideal for rooms where users don’t occupy fixed locations and can move freely throughout the space.
Deployment and Testing
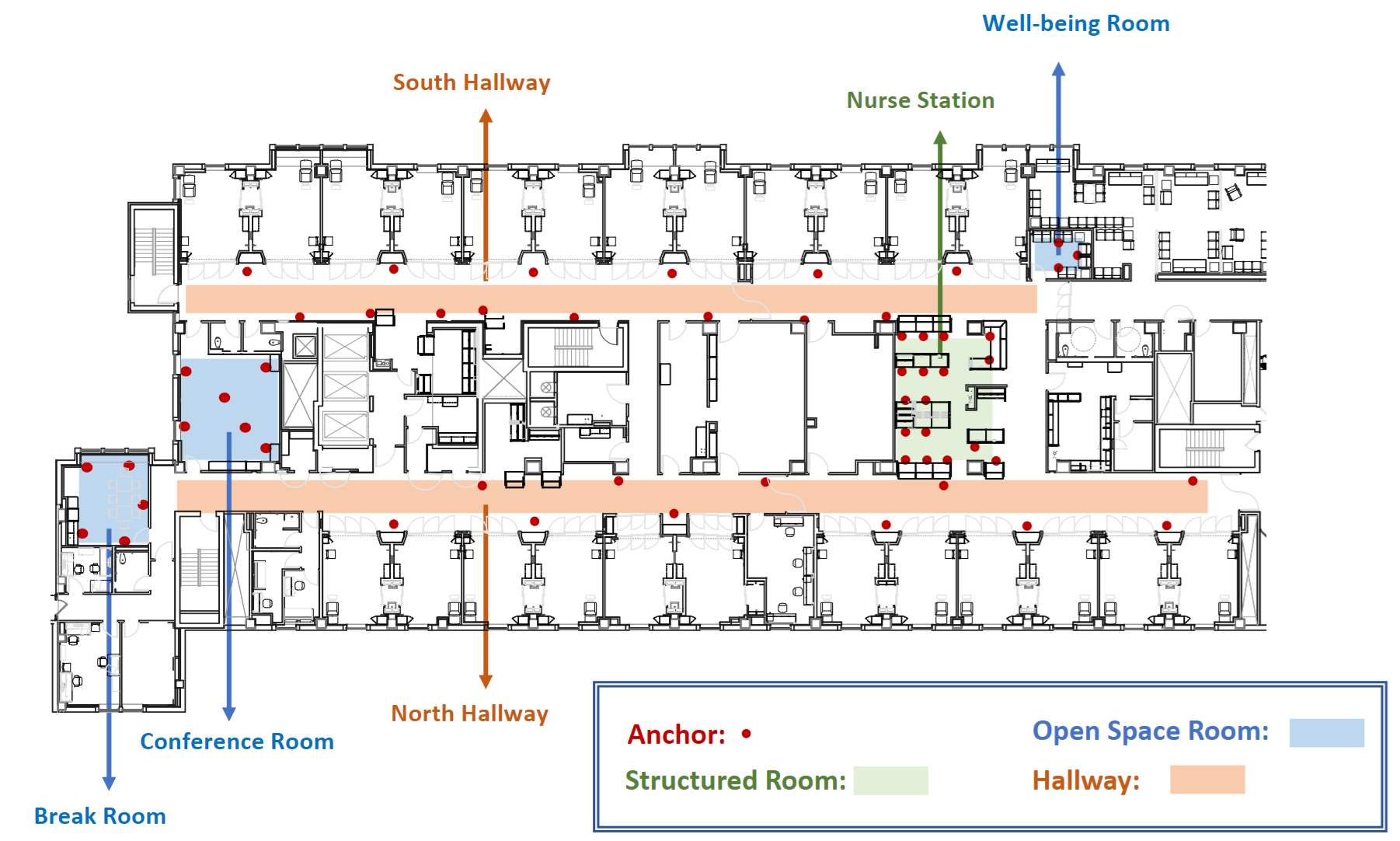
CATCH has been deployed in the ICU of a major medical center for testing, demonstrating high accuracy in detecting close contacts.
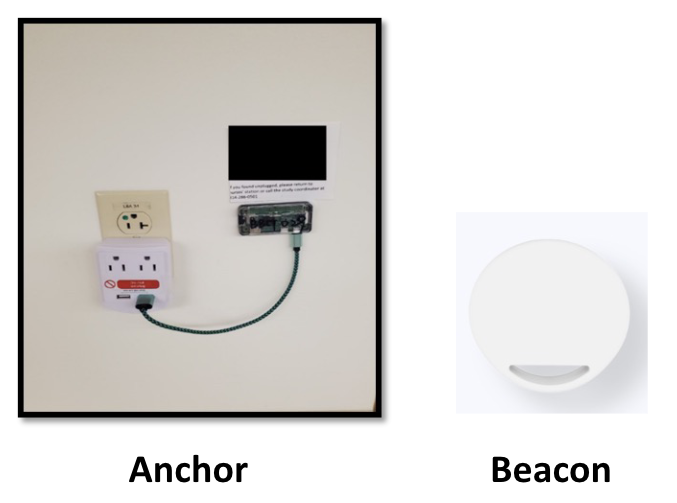
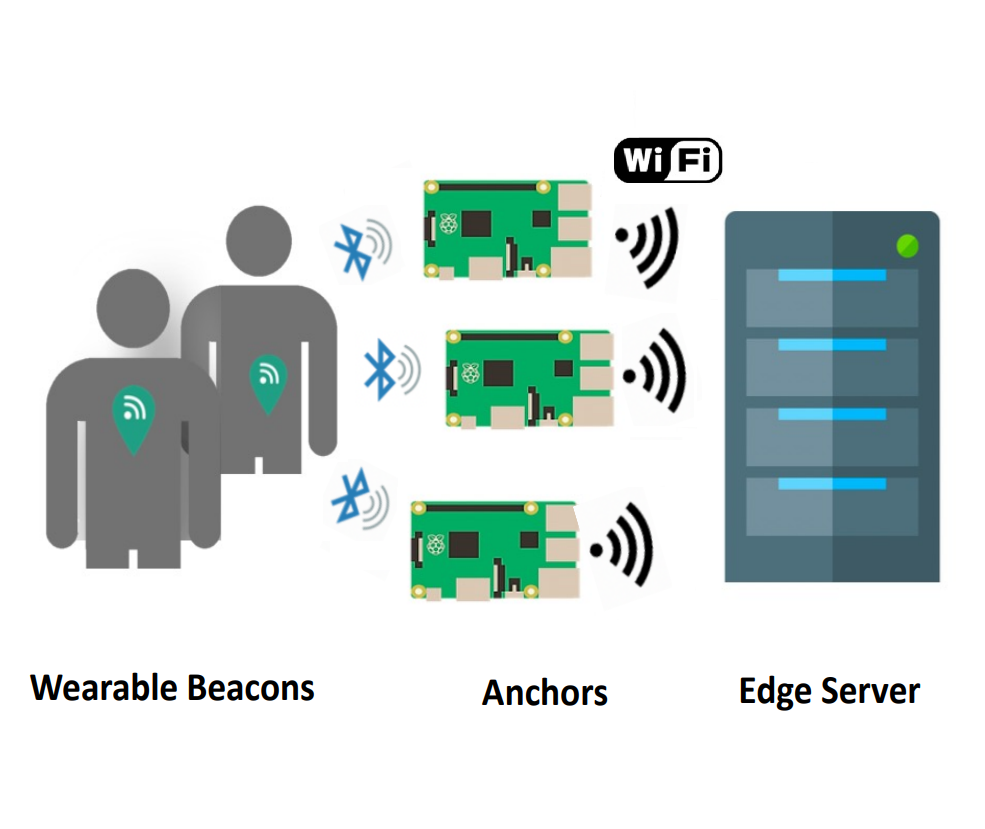
BLE Beacon Setup: Healthcare workers wear BLE beacons attached to their badges, broadcasting signals that nearby anchor devices (such as Raspberry Pi units) detect and relay to an edge server.
Anchor Device Placement: Anchors are strategically positioned throughout the ICU in hallways, structured rooms (e.g., nurse stations), and open spaces (e.g., break rooms) to ensure reliable coverage. Placement takes into account both room layouts and power availability.
Data Processing on Edge Server: An edge server gathers all beacon data from the anchors, running the contact tracing pipeline in real-time. The server also stores beacon messages in a secure, anonymized database for analysis, ensuring compliance with privacy regulations.
Results
Real-world testing validated the system’s advantages over manual tracing, with improved sensitivity and reliability in identifying contact events across varied ICU layouts.
| Method | Environment | Sensitivity | Specificity | Accuracy | F1 Score |
|---|---|---|---|---|---|
| Clustering | Hallways | 0.865 | 0.857 | 0.864 | 0.907 |
| Semantic Localization | Structured Rooms | 1.000 | 1.000 | 1.000 | 1.000 |
| Radio Fingerprint | Open Spaces | 0.895 | 0.851 | 0.880 | 0.909 |
Collaborators
- Washington University in St. Louis - AI for Health Institute
- Washington University in St. Louis - Cyber-Physical Systems Laboratory
- Washington University School of Medicine - Department of Medicine